Leah Riley, Histology Manager at Royal Devon and Exeter Hospital, explains why and how her team ditched paper and the issues they overcame on their journey to a greener laboratory.
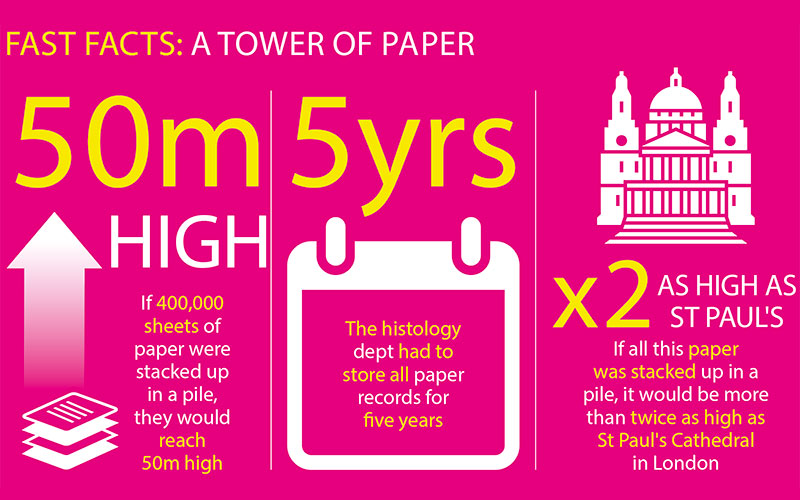
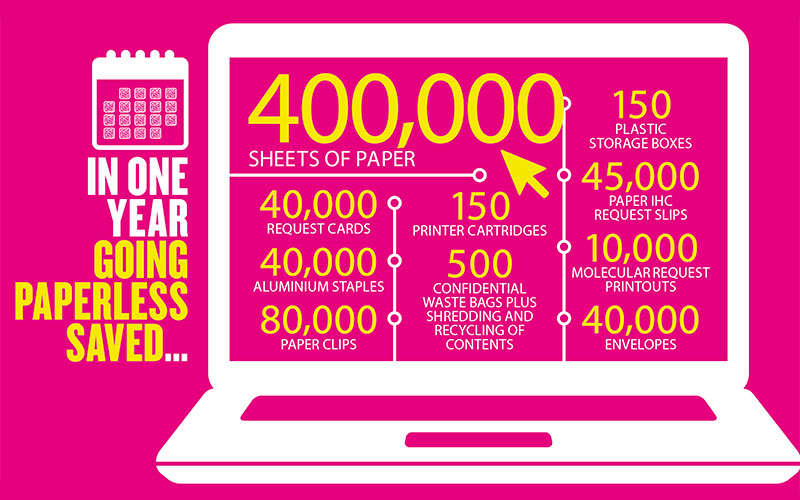
In 2018, as part of our green team initiative, the histology team began investigating paper usage within the department and how we could, as a laboratory, reduce the paper that we use and then discard. We calculated that in histology we used ~400,000 sheets of paper per year (which if stacked up would be nearly 50 metres tall) all of which needed to be stored for five years (by which time the stack would be more than twice as high as St Paul’s Cathedral) and then disposed of through our confidential waste pathway. (See the illustration, below, for the full breakdown.)
Our paper usage was phenomenal and the team were hindered by an aged LIMS system and the historic reliance upon paper. Trying to encourage people to give up paper was going to be a challenge; the comfort of a paper trail was firmly embedded into the day-to-day operations. The green team tried in vain to get people to relinquish their grip on paper by asking them to reduce printing of patient histories and carrying out report checks on screen. Unfortunately, we could not entice a majority to embrace such drastic changes and the paper shuffling continued.
We entered 2019 with high hopes and the scent of change was the catalyst for our revolution. The trust embarked on the procurement of a new electronic patient records system including a new LIMS system for histology. Finally we would be able to lay our 1989 LIMS system to rest and enter into the 21st century. The team was ready for change and had the enthusiasm to realise the potential for improving our green credentials in the process. Right from the beginning we discussed going paperless, which on occasion was met with a horrified glare and shrieks of “but how, how could I possibly give up my paper”. Let us begin our journey…
Request cards
Since the dawn of histology any specimen must arrive in the department with a request card so we can check the patient information to confirm that the request and pot match, if not, back it must go. Sound familiar? Beaker is the LIMS for EPIC Pathology and we were responsible for building our part of the system. If we no longer required, nor wanted, a request card, we needed a label, which could be scanned to view the request and clinical information on screen. We constructed a label that housed readable information and a 3D barcode, when upon scanning opened up the case and simultaneously gave the specimen its unique histology number. You then check the pot label against the screen and accept the specimen and label. It’s all too simple, you are thinking, well yes – you are reliant upon the label maker selecting the right specimen details, much akin to completing a legible request card. To encourage compliance, when building our system we found it was easier for the users to build a list of specimens that they want to select from, then we translated that into a histology-friendly format at our end. Getting clinicians to fill out the clinical details, for some areas, we found the only way to accomplish this was to put in compulsory questions that they must answer to complete their order. No request card required – 40,000 request cards gone.
Right, the small matter of ~400,000 sheets of paper plus entourage. To start the tree felling we would print the patient history and attach this to the request card before the specimen even reached cut-up. During dissection of specimens we used to record the details on the reverse of the request card or on paper attached to the card. The macro was then typed later onto the LIMS. Without a request card the simplest solution was to type the macro directly into Beaker. To speed things along we studiously built proformas in line with Royal College of Pathologists’ data set requirements. This enabled the person supporting cut-up to tab between fields to efficiently enter the data. No paper required. Images in dissection are carried out on our Pathlite camera and stored in Beaker alongslide the histology number for easy access. The blocks are created by scanning the pot and printing the required number directly from Beaker. The blocks were scanned and processed overnight as per timeless tradition. The histology early birds arrive the following morning and begin embedding; when they scan the block in Beaker a vast improvement was the ability for the macro to appear on the screen so any embedding instructions could be read as the block was tracked. No more sifting through request cards leaving waxy remains.
Traditional microtomy relied on a block, a slide and a pencil plus some choice language for unremoved staples and sutures. Without giving up on the latter to maintain some folk element we replaced the transcribing of the block details onto the slide with a scan and print of a label. Legible and xylene resistant, they are racked and stained on our stainer (Leica SPECTRA, for those interested). Upon completion the slides formerly entered the sorting area where bits of paper were reassembled with the slides in a dance for which no one really knew the steps. This has now been replaced with a quick scan of a slide to see, on screen, the required slides for the case to assemble them into a tray. The slides then go to quality control, where they are scanned (therefore, tracking them) and the macro checked microscopically against the description, assigned to a consultant pathologist, if appropriate, then delivered to the destination tray.
Just Some benefits of the new system
- No transcription errors between paper copy and typing – a previous audit revealed 5% of reports had transcription errors that were never identified
- Increased accuracy and precision
- No lost bits of paper
- No phone calls demanding a copy of the report – copies are added electronically
- Transparency of information – patients can also see parts of their reports on EPIC
- Audit trail – specimen tracking, the lab is no longer the single place slides are lost
- No handwriting interpretation to decipher
- No more paper – to store or discard therefore creating space, saving 40 trees per year
- Examining our workflow and optimisation
- Saved time in filing and refiling
- Reduced booking-in time.
Reports
In days gone by, pathologists then completed paper slips to request extra work, which were infallible and were never lost (suspiciously only in the lab)! This fail-proof system has now become electronic with the pathologists asking for levels, IHC, special stains and molecular genetics requests directly onto the block in Beaker. The request appears on an electronic list, the block is cut and the label now with the pathologists’ initials on applied to the slide. The initials help with a timely return to the correct requestor. No more lost request slips and denial of slide ownership, the tracking system, much like the eye of Sauron in Lord of the Rings, sees all.
The consultant pathologists then complete either a proforma report or free-text type the report directly into Beaker. A second consultant then validates and the report is released. I must point out that there is a mixture of typing and voice recognition for reporting. This electronic process has saved paper reports from being printed for checking and sending to the service user, plus the extra carbon copies to those requested. This process even works with ICE, so GP surgeries are able to access reports as soon as they are released by the pathologist. No lost reports in the post and urgent reports can be read instantly. This is particularly effective with intra-operative reporting of frozen sections. The surgeon has instant access to this report and nothing is lost in translation.
Positive change
Going paperless not only improved areas of the laboratory, but it really made us examine how the work flowed through the department (see list, above, for some other benefits). Like most laboratories we often don’t have that much space to spread ourselves out. By replacing the paper with technology we have re-organised our workflow. For example, why were we walking across the lab every time we needed to retrieve a block for levels? Let’s move the most current blocks to the workstation dealing with the extra request lists. Lean had once been an unspoken word in the lab – a system dictated by those who never regularly carried out the task involved and never considered happiness in the quota. Now we a have a workflow designed by the team for the team.
The comfort of a paper trail was firmly embedded into the day-to-day operations
I realise that we had the luxury and privilege of a new system that has enabled our move away from paper. However, this was driven by the team wanting to reduce our impact on the environment and early discussion built the unity to achieve this. If anything, add a green credential to your KPIs, quality management review or have a green champion to give your team a platform to put forward ideas and open a dialogue for discussion. It is now an agenda item and we aren’t just getting rid of paper, watch out plastics and unrecyclable packaging – you are next! Change is often good and positive and fear of change can be allayed by getting involved. The last 12 months since go-live of our new system has not been easy, but we have made it.