Why did a disease that is endemic in the tropical rainforest environments of West Africa and the Congo basin start spreading around the world?
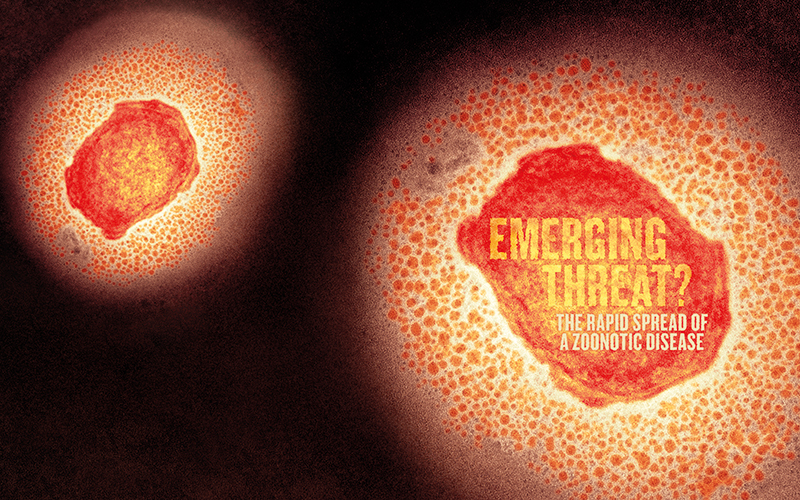
Monkeypox has made headlines over recent weeks not just for a rapid rise in numbers around the world, but for the very nature of its name. Just as this magazine was going to press, the Director-General of the World Health Organization (WHO) announced urgent efforts were underway to rename the disease. The WHO told the Biomedical Scientist it is “in discussion with experts and technical advisory groups in poxvirology and viral evolution on the possible renaming of monkeypox virus clades”. A spokesman said: “We will make announcements about the new names as soon as possible.” However, as the magazine went to the printers, the official name remained monkeypox (see box, left).
This latest outbreak of the zoonotic virus, an orthopoxvirus closely related to smallpox, is especially alarming, coming as it does so swiftly on the heels of COVID-19. Just as we are enjoying returning to the old certainties, the worldwide infectious disease response may be set to ramp up once again.
First identified
Monkeypox was first identified in 1958 following an outbreak among laboratory monkeys in Denmark. It turned out that the monkeys were not the reservoir for the virus, but the name stuck all the same. The actual reservoir remains something of a mystery, though the principal hosts are thought to be indigenous African rodents. While the disease is endemic in the tropical rainforest environments of West Africa and the Congo basin, it escaped that environment in 2003, when an outbreak in Wisconsin in the US that affected more than 70 people was traced back to imported Gambian pouched rats.
Several other outbreaks of monkeypox have occurred since then but have mostly been limited and short-lived. This latest episode is somewhat more significant in reach and scale. The first case was confirmed on 6 May in the UK – traced back to a patient who had recently travelled from Nigeria – though the virus’ often long incubation period means it may have been spreading for several weeks before that point. Since then, cases have been diagnosed across Europe, and in North and South America, and Australia. As at 17 June, they totalled more than 1880, with nearly 600 of those here in the UK.
Why rename monkeypox?
WHO said: “Human monkeypox was given its name before current best practices in naming diseases: names should be given with the aim to minimise unnecessary negative impact of disease names on trade, travel, tourism or animal welfare, and avoid causing offence to any cultural, social, national, regional, professional or ethnic groups.
“WHO is considering the name of monkeypox and whether to rename it. For a disease that already exists, the process would include consideration of the international classification of diseases (ICD-11).
“Naming of viruses is the responsibility of the International Committee on the Taxonomy of Viruses (ICTV). There was already a process underway to reconsider the naming of all orthopoxvirus species. This will continue under ICTV leadership.”
Symptoms
The symptoms of monkeypox are similar to those of its cousin virus, smallpox. It can incubate for anywhere between five days and 21 days, but most usually between six and 13 days, and the first symptoms are a fever, headache, muscular pain and fatigue. Though these are fairly general signs of illness, the more specific indication of monkeypox at this stage is swollen lymph nodes in the neck. After a few days of this comes the vesicular rash, usually starting on the face and then spreading to the rest of the body, particularly the palms of the hands and the soles of the feet, inside the mouth, on the genitals and even in the eyes. This rash, like that seen with smallpox, is composed of clusters of blisters or lesions filled with fluid that often burst before drying up and then scabbing over.
Though it sounds nasty, monkeypox is, in most cases, fairly mild and self-limiting, with symptoms clearing up after two to four weeks. However, for some people the disease can be a far more dangerous prospect. For the young and the old, people with compromised immune systems and pregnant women, it can cause lasting damage, such as birth defects and loss of vision, and complications from secondary infections, such as pneumonia, sepsis and encephalitis. The fatality rate for this current strain, which is believed to be the weaker West African variety, is expected to be around 3%.

The leap
Originally the disease would have been transmitted to humans when they came into contact with infected animals or, on occasion, ate infected meat. But now the virus has made that leap across the species, it’s spreading from human to human, though infection requires close, even intimate, contact. That means direct exposure to an infected person’s lesions, body fluids, coughs or sneezes. Contaminated surfaces are a typical route for infection, especially bedclothes, towels and other material that may have soaked up the virus-laden fluid released when the lesions rupture.
In the UK, many of the early cases have been among young homosexual and bisexual men in London. While monkeypox is not in itself a sexually transmitted disease, it does suggest that the intimacy of sexual activity may be a significant factor in the current spread of the infection. People who have everyday contact with these infected people, such as family members and healthcare workers, will also be at risk.
But at this early stage much of the recent outbreak remains a puzzle simply because it is so unprecedented. For a disease that was predictably restricted in the main to parts of Western and Central Africa, it has suddenly become very unpredictable. Why an outbreak now and why in so many different countries?
The outbreak
“In terms of why it’s spreading, I think several things may be going on here,” says Dr Sarah Pitt, principal lecturer in the School of Applied Sciences at the University of Brighton. “One of them is that outside of Africa, you just wouldn’t have been prepared for it. The public health authorities weren’t expecting an outbreak and it has taken them a while to start dealing with it.”
Something else that may have helped the spread is that, as with many infections, there is great variation in the severity of the symptoms. Some people develop a rash with lesions all over their body and some have only a few lesions. “It might be that some infected people had a couple of spots in areas where they weren’t aware of them and could have passed it on to others without really knowing about it,” says Pitt. Even if they were aware of a lesion they won’t necessarily have realised that it was monkeypox, given the disease’s relatively low profile up to this point.
“It’s now possible to go on a flight without having pre and post COVID tests, it’s logistically much easier”
Another potential factor is the restart of international travel, which noticeably took off again this spring. “It’s now possible to go on a flight without having pre and post COVID tests, it’s logistically much easier,” says Pitt. Along with the freedom of movement restored after the travel restrictions of COVID, other pandemic-imposed barriers may also have fallen. People have started having fun again and are perhaps throwing caution to the wind in the process. One theory suggests this outbreak is linked to sexual contact at recent European festivals.
Could COVID also have assisted this outbreak of monkeypox after so many immune system challenges during the past two years, leaving large numbers of people vulnerable to infections they might have otherwise shaken off? “Some 70% of people in the UK are expected to have had COVID,” says Pitt, “and we know that does potentially affect your immune system, even if you think you’ve fully recovered. It’s possible this outbreak might be linked to COVID in that way but it’s a moot point”.
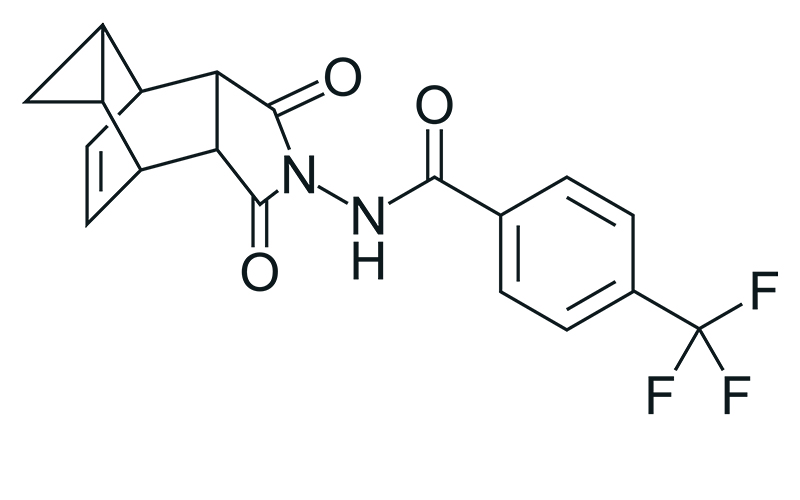
An antiviral agent, tecovirimat, developed to treat smallpox, has also been licensed to treat monkeypox
The new COVID?
With WHO and all the relevant national infectious disease agencies launching investigations, along with containment and treatment programmes, the real drivers behind this outbreak should become clear soon enough. For the time being, though, there is little need to worry that this is the new COVID, that pandemic restrictions are about to come slamming down again. “With COVID, flu and colds, the virus is largely airborne,” says Pitt. “An infected person can cough and sneeze and the virus hangs around in the air and then you can go to a supermarket or travel on a train and pick it up. Monkeypox is different because it requires that really close contact.”
The other key difference is that COVID was a novel virus, whereas monkeypox, related so closely to smallpox, which has plagued humanity for thousands of years, is well established. “We haven’t had any smallpox cases since 1980, but our immune systems, our genetic makeup, will still have something to work with against monkeypox,” says Pitt. “But the key problem with a lot of zoonotic diseases is that they are brand new in the human population. That’s part of what we saw early on with COVID, that massive overreaction of the immune system. It just didn’t know what to do with this new virus.”
Monkeypox – a timeline
- 1958 Monkeypox is first identified after an outbreak among laboratory macaques in Copenhagen.
- 1970 The first human case of monkeypox is recorded: a baby boy in the Democratic Republic of the Congo (DRC), Central Africa.
- 1970 onwards Human cases are reported in 11 countries across Central and Western Africa.
- 1981–86 More than 300 human cases are reported in the DRC, most a result of contact with animals. The fatality rate is around 10%.
- 1996–97 Another DRC outbreak, this time most cases are a result of human-to-human contact.
- 2003 The first outbreak outside of Africa occurs in the US. Around 70 people are infected, with no fatalities.
- 2017–19 Nigeria experiences an outbreak, with over 500 suspected cases and fatality rate of around 3%.
- 2018 The UK records its first case, a Nigerian national who travelled to the country.
- 2019 A case emerges in Singapore – another traveller from Nigeria.
- May–June 2022 A new case emerges in the UK. Multiple cases follow in more than 20 non-endemic countries. Studies are launched to understand infection and transmission. WHO warns the disease may become endemic outside Africa. The question of the true burden of the disease is unanswered.
Zoonotic threats
This points to the underlying and ever-growing threat from new zoonotic diseases. While monkeypox is not necessarily that threat, others certainly are lurking around the corner. The ongoing depletion of natural habitats, putting humans in closer contact with wild animal populations, is a clear factor in raising the risk of novel zoonotic pathogens, whether viral, bacterial or parasitic. So too is the burgeoning global agricultural sector, where industrial quantities of livestock are giving rise to antimicrobial resistance, affording pathogens new opportunities to exploit and flourish, and to make the jump over to human hosts. Mass-scale food production processes also pose a risk, as do the more traditional and less-ordered meat markets that trade in wild animals – though the investigation into the spillover event for COVID remains inconclusive, a key venue for that pivotal moment remains such a market in Wuhan, China.
As COVID has amply demonstrated over the past few years, any novel zoonosis brings with it the potential for an epidemic, exacerbated by a lack of effective treatment and prevention, triggering enormous social, economic and political consequences, and causing millions of deaths.
“I think all this just goes to show how important surveillance is,” says Pitt. Pre-COVID, there may have been a sense that infectious diseases wreaking havoc on a global scale were a shrinking problem, that public health and vaccine programmes had effectively dealt with them, and that the true challenge for medical science, and the best investment for precious resources, was now the burden of non-infectious genetic and lifestyle disease, such as cancer, diabetes and cardiovascular conditions. “And so we took our eye off the ball,” says Pitt.

Outbreak response
Sequencing of virus isolates from the current outbreak of monkeypox indicates it’s the milder West African strain rather than the stronger Central African version.
Vaccines used to eradicate smallpox have also provided protection against monkeypox. A new smallpox vaccine was licensed in 2019 and has been approved to prevent monkeypox.
An antiviral agent, tecovirimat, developed to treat smallpox, has also been licensed to treat monkeypox. This drug inhibits the activity of the VP37 viral envelope protein, preventing the production of progeny virus from an infected cell.
Keep vigilant
The emergence of monkeypox at this time simply reinforces the point, as if it were needed, that infectious diseases have not gone away and are highly unlikely to do so in the foreseeable future.
“We’ve been rather good at controlling viruses and bacteria with vaccines and antibiotics and so on,” says Pitt. “A lot of lives have been saved over the past 100 years and people’s quality of life has also improved as a result of these measures. But we have to keep vigilant. COVID and this latest outbreak of monkeypox have highlighted just how important that vigilance is. Governments cannot afford to think the job is done. They have to invest in training scientists, in equipment, in sequencing capacity, in laboratory space and facilities, in everything that helps us deal with these diseases.”
Image credit | Science-Photo-Library | Shutterstock | iStock